Naviscreen-Hb
Haemoglobinopathies
Haemoglobinopathies, i.e., the hereditary hemoglobin disorders, in particular SICKLE CELL disease and Beta- Thalassemia are the most common, preventable, genetic disorders inherited from parents to their kids i.e. The abnormal gene is passed on from one generation to another, in INDIA, which are associated with chronic, life impairing and life-threatening health problems and can lead to disability and death, imposing a heavy social and economic burden on both the families and the government resources.
These disorders often show symptoms early childhood and, although lifelong in nature, can be better managed if identified early through screening. Many carriers have no symptoms but may pass the condition on to their children, leading to potential health risks that can be addressed through informed counselling and medical follow-up.
They are equally prevalent in males and females
Have a ‘carrier’ Silent or very few symptoms and can be detected by screening tests ‘disease’ state or severely symptomatic life threatening.
A couple where both the partners are carriers of an abnormal gene (mutated gene) have
- 25% risk to have a child with disease state
- have 25% chance of having a ‘normal’ child
- have a 50% chance to give birth to a ‘carrier’ child
Clinically Relevant and Types
Haemoglobinopathies affect Hemoglobin—the protein in red blood cells responsible for carrying oxygen throughout the body. Clinically significant hemoglobinopathies arise from point mutations or gene deletions.
People with these conditions may produce hemoglobin that’s structurally abnormal (such as sickle cell disease, where cells become crescent-shaped and fragile) or made in reduced amounts (as seen in Thalassemia), causing anemia, fatigue, pain episodes, and sometimes organ damage.
Disease occurs in homozygous or compoundheterozygous states—e.g. Hb SS, Hb S / βthalassemia, Hb E/βthalassemia, and Hb H disease—leading to hemolysis, anemia, vasoocclusion, organ damage, and transfusion necessity. Although many carriers remain asymptomatic, early identification enables counseling, prevention of complications, and therapeutic intervention.
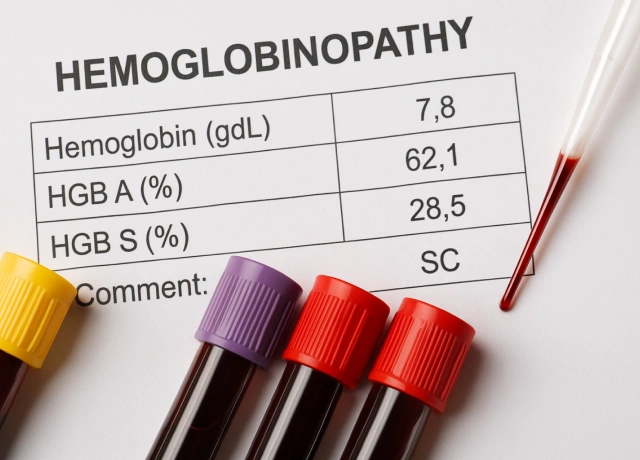
| Hemoglobinopathy | Affected Globin Chains | Mutation Type | Symptoms | % of Hb in Adults/Children |
|---|---|---|---|---|
| Sickle Cell Disease (SCD) | α₂β₂ (HbS) | Point mutation (Glu6Val in β-globin) | Pain crises, anemia, jaundice, stroke risk | HbS (80-95%) in SCD, 35-40% in trait, HbA absent in homozygous |
| Hemoglobin C Disease | α₂β₂ (HbC) | Point mutation (Glu6Lys in β-globin) | Mild anemia, splenomegaly | HbC (90-98%) in disease, 35-40% in trait |
| Hemoglobin SC Disease | α₂β₂ (HbSC) | Compound heterozygous (HbS & HbC) | Vaso-occlusive pain, anemia, splenomegaly | HbS (50%), HbC (50%), no HbA |
| Hemoglobin E Disease | α₂β₂ (HbE) | Point mutation (Glu26Lys in β-globin) | Microcytosis, mild anemia | HbE (85-95%) in disease, 30-40% in trait |
| Hemoglobin D Punjab | α₂β₂ (HbD Punjab) | Point mutation (Glu121Gln in β-globin) | Mild anemia, possible splenomegaly | HbD (95-100%) in disease, 35-40% in trait |
| Beta-Thalassemia Major (Cooley’s Anemia) | α₂β₀/β₀ or α₂β⁺/β⁺ | Deletion/point mutation reducing β-globin production | Growth retardation, jaundice, hepatosplenomegaly, iron overload | HbF (80-100%) in disease, HbA absent |
| Alpha-Thalassemia Major (Hb Bart’s hydrops fetalis) | (–/–, –/–) (Hb Bart’s: γ₄) | Deletion of all four α-globin genes | Severe fetal edema, heart failure, stillbirth | Hb Bart’s (γ₄) >80% in disease |
| Hemoglobin H Disease | (–/–, –/α) (HbH: β₄) | Deletion of three α-globin genes | Anemia, jaundice, splenomegaly | HbH (β₄) 5-40% in disease |
| Hereditary Persistence of Fetal Hemoglobin (HPFH) | α₂γ₂ (HbF persistence) | Mutations increasing γ-globin expression | Often asymptomatic, protection against sickling | HbF (20-100% depending on mutation) |
Epidemiology
Tribal populations in Africa, India, and the Middle East can show up to 40% sickle cell trait, with 2–3% having the disease. Beta-Thalassemia is prevalent across India, with an average frequency of carriers being 3-4%. India accounts for 10% of global cases of Beta-Thalassemia and has the largest number of children with Beta-Thalassemia Major in the world (about 1-1.5 lakhs).
An estimated 10000-15000 babies with Thalassemia Major (TM) are born every year in India and about 42 million silent carriers of Beta Thalassemia Traits are there in India
Sickle Cell Anemia is highly prevalent in the tribal populations of Southern, Central and Western states of India, reaching as high as 48% in some communities. The prevalence of Sickle Cell Trait and Sickle Cell disease varies from 1–40% and 1–12%, respectively, in Indian tribal populations.
Other Hemoglobinopathies such as HbE disorder are highly prevalent in eastern part of the country and has a carrier frequency as high as 41%-66.7%. Permutations and combinations of these (i.e compound heterozygous cases) are also prevalent in India.
Disease Management
People with sickle cell disease (SCD)start to have signs of the disease during the first year of life, usually around 5 months of age. Symptoms and complications of SCD are different for each person and can range from mild to severe. SCD is a disease that worsens over time. Treatments are available that can prevent complications and lengthen the lives of those who have this condition. These treatment options can be different for each person depending on the symptoms and severity.
Primary strategy for management includes
Carriers are typically asymptomatic and require no medical interventions beyond ensuring adequate folate intake. The most critical management is reproductive planning—offer genetic counselling and prenatal or neonatal screening to prevent birth of children with severe homozygous or compound heterozygous haemoglobinopathies.
For diseases patients following are the main stay of Management
- Hydroxyurea to raise HbF and reduce pain crises in Sickle cell disease
- Maintaining haemoglobin at ~9–10 g/dL via regular packed RBC transfusions (typically every 3–5 weeks), in tandem with iron chelation therapy
- Rapid treatment of vasoocclusive crises (including simple or exchange transfusion when needed).
- Supportive care includes antibiotic prophylaxis and routine immunizations, monitoring organ function.
- Curative options include Bone marrow transplant or CRISPRbased gene therapy under clinical protocols.
What is Naviscreen-Hb?
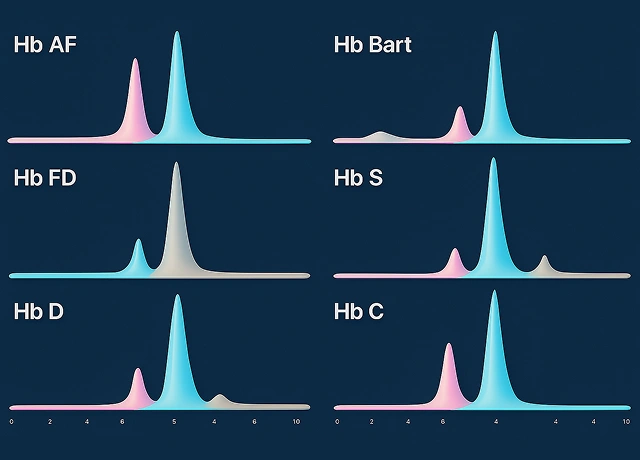
Naviscreen Hb is One Step Screening & Confirmation for all clinically relevant Hemoglobinopathies. This is a validated protocol: capillary blood is collected onto driedbloodspot (DBS) cards, followed by confirmatory testing using highperformance liquid chromatography (HPLC). HPLC remains the internationally accepted gold standard for diagnosing hemoglobinopathies such as sickle cell disease, Hb E, and βthalassemia.

Validated
Naviscreen-Hb is ICMR (Indian Council of Medical Research) validated and NABL (National Accreditation Board for Testing and Calibration Laboratories) accredited protocol. It is also accredited by ACCAB and has been published in Indian Journal of Public Health
| Logo | Certificate / Accreditation |
|---|---|
|
ICMR (Indian Council of Medical Research) validated protocol for Naviscreen-Hb. |
|
NABL (National Accreditation Board for Testing and Calibration Laboratories) accredited method. |
|
ACCAB (Accreditation Commission for Conformity Assessment Bodies) accredited protocol. |

Experience
Navigene has established worldclass diagnostics for haemoglobinopathies through alliances with over 500 hospital partners across India, besides serving governmentrun publichealth programs. Leveraging validated DBSHPLC methodology, the company has consecutively delivered massscreening across more than 30 districts in Chhattisgarh and Odisha—completing over 1.5 million individual tests. The Cuttack facility, the largest dedicated HPLC laboratory in the region, was instituted to ensure highthroughput reliability in hemoglobin variant quantification and is fully NABLaccredited.
How to avail the test?
Step 1 : Register
Register for Naviscreen-Hb and select the package you want for your baby in consultation with your doctor or Navigene Experts.
Sampling
Based on the package selected, collect the Urine and/or Blood sample on the special collection kits provided at time of registration and send it to Navigene or call us for a pickup (A Navigene partner hospital will do this for you.
Results
Navigene will send a comprehensive and easily interpretable report within 1-2 days followed by any assistance as required.
Frequently Asked Questions
What does “carrier” (trait) mean in hemoglobinopathies?
Having one mutated α or βglobin gene (e.g. sickle or βthalassemia trait), carriers are usually asymptomatic, and rarely require treatment or follow-up
How do symptoms differ between carriers and individuals with disease
Carriers are asymptomatic; individuals with two pathogenic alleles (e.g., HbSS, βthalassemia major) typically exhibit chronic hemolysis, severe anemia, pain crises, growth delays, and organ complications.
How can families avoid passing on hemoglobinopathies to the next generation?
Through genetic counselling and partner testing—concordant carrier couples have a 25% chance of an affected child, and may consider prenatal diagnosis or assisted reproduction.
Who should be tested for hemoglobinopathy traits or disease?
All individuals from highrisk populations or those with family history—as well as all pregnant women and their partners, ideally before 10–12 weeks gestation.
Is it acceptable to test before pregnancy?
Yes—preconception carrier screening allows informed family planning and avoids surprises later in pregnancy.
Can hemoglobinopathies be cured?
Curative options include allogeneic hematopoietic stem cell transplantation for matchedsibling donors, and emerging CRISPR/lentiviral gene therapies like Casgevy (FDA/MHRA-approved for SCD and transfusiondependent βthalassemia).
What treatments are available for those affected?
Standard management includes hydroxyurea, regular transfusion (for βthalassaemia major or sickle crises), iron chelation, folic acid, vaccinations, and routine specialist followup.
What should one do after learning they are a carrier?
Seek genetic counselling, inform and screen partner, calculate reproductive risk, and consider prenatal testing or alternative reproductive options.
Is genetic counselling recommended after a positive result (trait or disease)?
Yes—counselling improves understanding, relieves anxiety, and guides reproductive decisions among couples with risk of hemoglobinopathy births.
Who collects the sample?
A trained staff will collect the sample. This can often be done by a Navigene partner hospital. Or you can also take your own sample after following the steps mentioned in DBS card or see the link for a video demonstration
Is DBS screening accurate and reliable?
Yes—studies in newborn/field settings show ~100% concordance between DBSHPLC and standard venous blood HPLC for clinically significant variants.
How often should diagnosed individuals be monitored?
Routine followup is vital—every 3 months for SCD, to monitor growth, anemia, iron overload, prevent complications, and adjust therapy; βthalassaemia major requires lifelong monitoring





